Objective: this work seeks to complement and extend prior work by using a multidisciplinary approach to explain electronic medical records (emr) system use and consequent performance (here, patient satisfaction) among physicians during early stages of the implementation of an emr. design: this was a quantitative study, with data obtained from three distinct sources: individual-level and social. Jan 1, 2019 the emr or electronic medical record refers to emr of use everything you'd find in a paper chart, such as medical history, diagnoses, medications, . The electronic medical record (emr) is an enabling technology that allows physician practices to pursue more powerful quality improvement programs than is possible with paper-based records.
Faststats Electronic Medical Records
The key barriers to physicians' use of emrs include high initial costs and uncertain financial benefits; high initial physician time costs to learn the system; . Without it, meaningful use of ehr technology simply isn’t possible. here, we’ve put together five effective ehr training tips to get staff in your practice adequately trained and comfortable on a new system: 1. identify employee computer skills and provide basic training. it should be noted that some european countries use the age of 16 rather than 8 this helps convey the dangers of emr even in these amounts, especially to young people The electronic medical record (emr) is an enabling technology that allows physician practices to pursue more powerful quality improvement programs than is .
An ehr and an emr vary greatly, although many use the terms ehr and emr interchangeably. an emr (electronic medical record) is a digital version of a chart with patient information stored in a computer and an ehr (electronic health record) is a digital record of health information. differences between ehr and emr. Advantages of electronic health records. ehrs and the ability to exchange health information electronically can help you provide higher quality and safer care for patients while creating tangible enhancements for your organization. ehrs help providers better manage care for patients and provide better health care by: providing accurate, up-to-date, and complete information about patients at. Feb 16, 2017 emr applications can also boost the quality and safety of patient care. with an emr system, you can prescribe and order medication for patients .

Some people use the terms “electronic medical record” and “electronic health record” (or “emr” and “ehr”) interchangeably. but here at the office of the national coordinator for health information technology (onc), you’ll notice we use electronic health record or ehr almost exclusively. Background: electronic medical record (emr) adoption in primary care has grown exponentially since their introduction in the 1970s. however, without their proper use benefits cannot be achieved. this includes: 1) the complete and safe documentation of patient information; 2) improved coordination of care; 3) reduced errors and 4) more involved.
The Use Of Electronic Medical Records Communication Patterns In
An ehr, or an electronic health record, is a digital version of a person’s overall medical history. ehrs are maintained by one provider, but can be shared to specialists and other medical caregivers when needed to maintain accurate information. 25 reasons why you need to use an emr 1. instant data retrieval. emrs let you find the data you need emr of use in literal seconds. there’s no more waiting around for 2. manage your personal schedule and work calendar. a good ehr offers time management tools. more efficient time 3. take and save. An electronic health record (ehr) is more than a digital version of a patient’s paper chart. ehrs are real-time, patient-centered records that make information available instantly and securely to authorized users. while an ehr does contain the medical and treatment histories of patients, an ehr system is built to go beyond standard clinical data collected in a provider’s office and can be. The emr system enables physicians to record patient histories, display test results, write prescriptions, enter orders, receive clinical reminders, use decision .

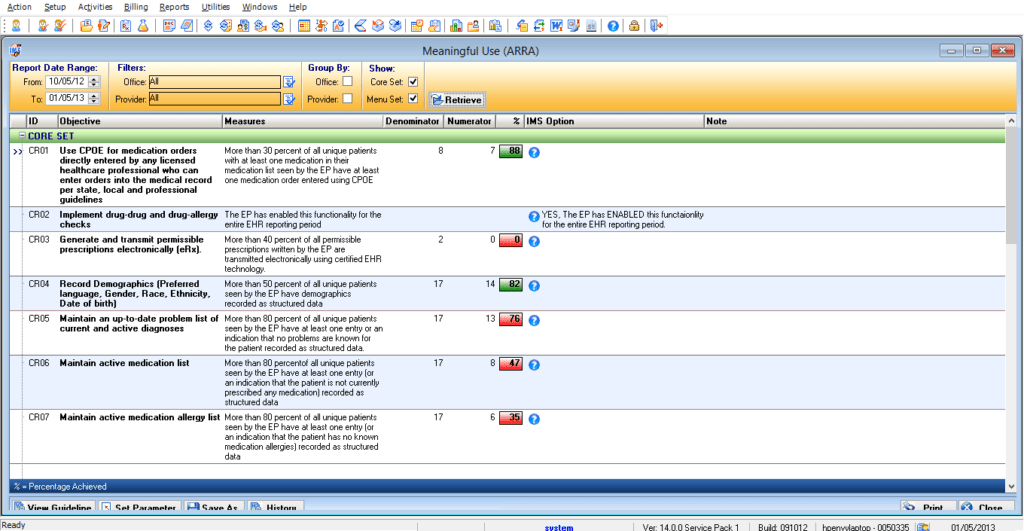
Percent of office-based physicians using any emr/ehr system: 85. 9%; percent of office-based physicians with a certified emr/ehr system: 79. 7%; source: percentage of office-based physicians using any electronic health record (ehr)/electronic medical record (emr) system and physicians that have a certified ehr/emr system, by u. s. state: national electronic health records survey, 2017 pdf icon. This guidance is intended to assist sponsors, clinical investigators, contract research organizations, institutional review boards (irbs), and other interested parties on the use of electronic. The electronic medical records (emr) mandate requires healthcare providers to convert all medical charts to a digital format. additionally, it’s a condition under the american recovery and reinvestment act (arra), whose objective is to incentivize and fund healthcare professionals using emr.
Benefits of emrs for clinics: · the emr automatically checks for problems whenever a new medication is prescribed to a patient and alerts potential conflicts with . Background: electronic medical record (emr) adoption in primary care has grown exponentially since their introduction in the 1970s. however, without their proper use benefits cannot be achieved. this includes: 1) the complete and safe documentation of emr of use patient information; 2) improved coordination of care; 3) reduced errors and 4) more involved patients. With an emr, that won’t be a problem anymore. 21. let’s you move around in your clinic. for many doctors, moving around the clinic is a huge part of their job. being able to use a mobile emr not only cuts down time for checking files, it also lets you input data right on the spot.
Emr Vs Ehr What Is The Difference Health It Buzz
The emr mandate explained. within arra, the health information technology for economic and clinical health act (hitech act) motivates health care organizations to implement emr. additionally, the government’s push toward the use of emr was created to make health records more accurate and accessible. One of the grand promises of health care digitization through the adoption of ehrs was better quality reporting and a path to improving day-to-day clinical outcomes by reinforcing best practices and modifying poor-quality care. 1,2 the move from vision to reality is not as simple as we would like, however. 3,4 to capture and leverage ehr content, the challenges relate to variability in the. As a part of the american recovery and emr of use reinvestment act, all public and private healthcare providers and other eligible professionals (ep) were required to adopt and demonstrate “meaningful use” of electronic medical records (emr) by january 1, 2014 in order to maintain their existing medicaid and medicare reimbursement levels. since that date, the use of electronic medical and health.
An electronic health record is the modern day, digital version, of a patient's paper chart. ehr systems provide real-time, patient-centered records that are instant, . Ehr systems are generally maintained by health care providers, health care organizations, and health care institutions and are used to deliver care. ehr systems can be used to integrate real-time. Mitigating the main issues surrounding ehr use is a challenge, but shifting data-entry tasks away from overburdened physicians and staff is a start. other experts think emr vendors will have to look beyond a patch for the problem. riggins says tech giants entering the healthcare space will make waves:. With meaningful use, including standard and consistent data entry in specific fields, the emr data provide the physician with valuable practice-level information.